WHY YOU NEED EMERGE AND SEE
Lost revenue often results from inconsistent billing workflows, missed follow-up, or unresolved payer activity. Our billing team manages claims processes and payer communication to help keep reimbursement organized and on track.

Delays in enrollment often result from incomplete applications, missed details, or payer-specific requirements. Our enrollment team manages applications and payer coordination to help providers become credentialed without unnecessary delays.

Many healthcare organizations require primary source verification to meet regulatory and accreditation standards. We verify provider qualifications and credentials to support participation, staff membership, and ongoing organizational compliance.

Ongoing credential maintenance is required to retain payer participation and facility privileges. We monitor credentials and manage updates to help prevent lapses that could disrupt access or reimbursement long term across organizations and care delivery environments.

WHAT WE DO FOR YOU
BILLING & REVENUE SUPPORT
We manage billing and claims workflows to support timely, accurate reimbursement and consistent payer follow-through.

DATA COLLECTION
We guide your practice administrators and providers in gathering all required information needed for most applications.

PAYOR COMMUNICATION
We do all follow-up and verification with each individual payer. All status updates are maintained in your secure cloud folder.
APPLICATION SUBMISSIONS
Once all required documentation is received, we complete, assemble and submit all required applications to individual payers.

EXPIRATION MANAGEMENT
We stay on top of all expirations in order to ensure a seamless process and up to date maintenance of all documentation.

CAQH ENROLLMENT
We complete and maintain CAQH applications required for provider credentialing with payors.
WHO WE PROVIDE CREDENTIALING SERVICES FOR






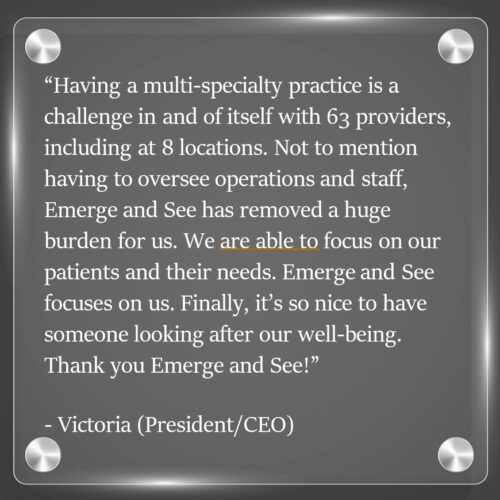
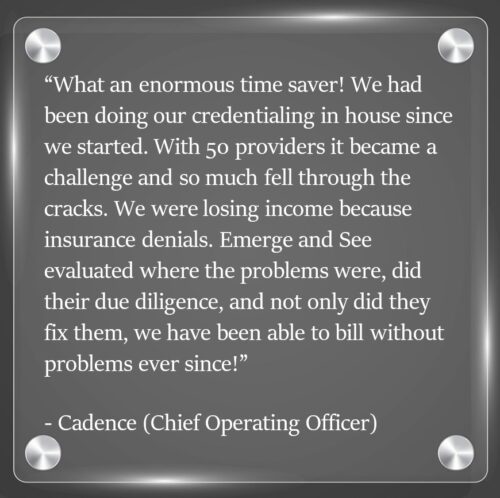
Emerge and See serves healthcare providers and facilities nationwide as a full-service billing and credentialing department. We support hospitals, federally qualified health centers (FQHCs), surgery centers, and healthcare organizations of all sizes, as well as physicians and advanced practice providers across diverse care settings.
Our teams manage comprehensive billing operations alongside provider and facility enrollment, recredentialing, and ongoing maintenance. We operate as an extension of your organization, ensuring billing workflows, payer participation, credentials, and privileges remain current, organized, and compliant. Our work is backed by a long-standing reputation for accuracy, consistency, and accountability.
Emerge and See is led by a healthcare administrator who understands the operational realities faced by leadership teams. That perspective shapes our white-glove approach—removing administrative burden from your shoulders, streamlining complex processes, and supporting the financial and operational goals of your organization so your team can remain focused on patient care and the bottom line.
Why Choose Us?
We treat each practice as if it is our own. We strive to please and ensure that you are ALWAYS happy with our services.
We tailor our services to fit your needs at all times. No two practices and/or specialties are the same. So why should our services be?
With over 20 years of experience and always staying up to date on the latest trends and technologies for credentialing services, we never miss a beat, so that you and your patients don’t either.
Our Credentialing Specialists are always there to serve you, your patients and the best interest of your practice. Your own, dedicated Account Manager will always be there to handle your specific needs.
Nationwide Medicaid Enrollment
Alabama – Alabama Medicaid
Alaska – Alaska Medicaid
Arizona – AHCCCS
Arkansas – Arkansas Medicaid
California – Medi-Cal
Colorado – Health First Colorado
Connecticut – HUSKY Health
Delaware – Delaware Medicaid
Florida – Florida Medicaid
Georgia – Georgia Medicaid
Hawaii – Med-QUEST
Idaho – Idaho Medicaid
Illinois – Illinois Medicaid
Indiana – Hoosier Healthwise
Iowa – Iowa Medicaid
Kansas – KanCare
Kentucky – Kentucky Medicaid
Louisiana – Louisiana Medicaid
Maine – MaineCare
Maryland – Maryland Medicaid
Massachusetts – MassHealth
Michigan – Michigan Medicaid
Minnesota – Medical Assistance
Mississippi – Mississippi Medicaid
Missouri – MO HealthNet
Montana – Montana Medicaid
Nebraska – Nebraska Medicaid
Nevada – Nevada Medicaid
New Hampshire – NH Medicaid
New Jersey – NJ FamilyCare
New Mexico – Centennial Care
New York – NY Medicaid
North Carolina – NC Medicaid
North Dakota – ND Medicaid
Ohio – Ohio Medicaid
Oklahoma – SoonerCare
Oregon – Oregon Health Plan
Pennsylvania – Medical Assistance (MA)
Rhode Island – RI Medicaid
South Carolina – Healthy Connections
South Dakota – SD Medicaid
Tennessee – TennCare
Texas – Texas Medicaid
Utah – Utah Medicaid
Vermont – Green Mountain Care
Virginia – Virginia Medicaid
Washington – Apple Health
West Virginia – WV Medicaid
Wisconsin – BadgerCare Plus
Wyoming – Wyoming Medicaid
The Value of an Embedded Partner...
Reduced administrative burden
Streamlined enrollment and billing workflows
Consistent, process-driven support
Scalable services as your practice grows